aacn CCRN-ADULT Exam Questions
Questions for the CCRN-ADULT were updated on : Feb 20 ,2026
Page 1 out of 10. Viewing questions 1-15 out of 150
Question 1
Assessment of a patient with a head injury reveals increased muscle tone and contractured
positioning of the upper extremities. A nurse should
- A. use wrist restraints to maintain upper extremity extension.
- B. obtain an order for a muscle relaxer.
- C. recognize that contractures are an expected response after a head injury.
- D. consult a physical therapist regarding appropriate positioning.
Answer:
D
Explanation:
In patients with head injuries, increased muscle tone and contractured positioning (such as
decorticate or decerebrate posturing) are signs of significant neurological impairment. It is essential
to manage these symptoms to prevent further complications. Consulting a physical therapist is the
best course of action to ensure appropriate positioning, prevent contractures, and manage spasticity
effectively. Reference: = CCRN Exam Handbook and AACN's Certification Review Course materials.
Question 2
A patient was admitted 3 days ago for an overdose of acetaminophen (Tylenol). The patient is
developing a decreasing level of consciousness. Which the following is the most likely finding?
- A. Cheyne-Stokes respirations
- B. splenomegaly
- C. decreased GFR
- D. increased INR
Answer:
D
Explanation:
A patient with acetaminophen overdose is at risk for acute liver failure, which can lead to
coagulopathy. This condition is often marked by an increased International Normalized Ratio (INR)
due to impaired synthesis of clotting factors in the liver. Decreasing level of consciousness can also
result from hepatic encephalopathy, a complication of liver failure. Reference: = CCRN Exam
Handbook and AACN's Certification Review Course materials.
Question 3
Which of the following diagnostic procedures best pinpoints the location, size, and origin of a
cerebral aneurysm?
- A. MRI
- B. cerebral angiography
- C. positron emission tomography (PET) scanning
- D. CT scanning
Answer:
B
Explanation:
Cerebral angiography is considered the gold standard for diagnosing and pinpointing the location,
size, and origin of cerebral aneurysms. It involves the use of contrast material injected into the
cerebral arteries and imaging to provide detailed visualization of the blood vessels in the brain,
which is essential for accurate diagnosis and planning treatment strategies. Reference: = CCRN Exam
Handbook and AACN's Certification Review Course materials.
Question 4
A patient is experiencing lower left quadrant pain with guarding, as well as abdominal distention and
rigidity. KUB reveals free air in the abdominal
cavity. Vital signs are:
BP
76/40
HR
130
RR
T
101.7° F (38.7°C)
A nurse would suspect
- A. perforated bowel.
- B. paralytic ileus.
- C. appendicitis.
- D. acute pancreatitis.
Answer:
A
Explanation:
The clinical presentation of lower left quadrant pain with guarding, abdominal distention, rigidity,
and free air in the abdominal cavity on a KUB (kidney, ureter, and bladder) radiograph strongly
suggests a perforated bowel. The presence of free air indicates that there is a breach in the
gastrointestinal tract, allowing air to escape into the peritoneal cavity. The patient's vital signs,
including hypotension (BP 76/40), tachycardia (HR 130), tachypnea (RR 32), and fever (T 101.7°F), are
consistent with sepsis and shock, which are common complications of bowel perforation. Reference:
CCRN Exam Handbook, AACN, page 30, section on Gastrointestinal.
Question 5
A patient with an acute anterior wall MI presents with an S3 gallop and the following values: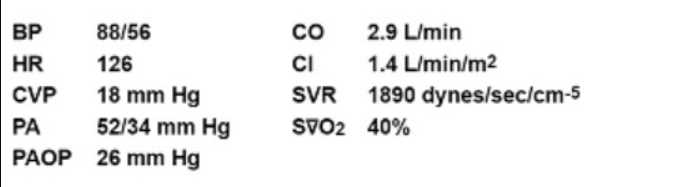
Which drug therapy would be most appropriate for this patient?
- A. vasodilators and positive inotropes
- B. vasopressors and beta-blockers
- C. vasodilators and diuretics
- D. vasopressors and calcium-channel blockers
Answer:
C
Explanation:
In the setting of an acute anterior wall myocardial infarction (MI) with an S3 gallop, the patient is
likely experiencing heart failure and possibly acute pulmonary edema. The appropriate treatment
includes vasodilators to reduce afterload and diuretics to decrease preload and pulmonary
congestion. This combination helps to improve cardiac output and reduce the workload on the heart.
Reference: CCRN Exam Handbook, AACN, page 20, section on Cardiovascular.
Question 6
A patient post-surgical externalized ventricular drain placement has treatment orders that include
continuous cerebrospinal fluid (CSF) drainage at 10 mm
Hg. Which of the following should the nurse anticipate with an increase in the ICP above 25 mm Hg?
- A. a decrease in the pulse pressure
- B. a change in CSF drainage from clear to pink
- C. the amplitude of P2 greater than P1 on the waveform morphology
- D. an increase in the cerebral perfusion pressure from 65 to 70
Answer:
C
Explanation:
An increase in intracranial pressure (ICP) above 25 mm Hg often results in changes in the waveform
morphology observed in the monitoring of intracranial pressure. Specifically, the amplitude of P2
becomes greater than P1, which is indicative of decreased intracranial compliance. This pattern is
known as the "pathological waveform," suggesting increased intracranial pressure and decreased
ability of the brain to accommodate the pressure changes. Reference: CCRN Exam Handbook, AACN,
page 23, section on Neurological.
Question 7
The dysrhythmia most commonly associated with mitral stenosis is
- A. second-degree AV heart block, Mobitz Type II.
- B. idioventricular rhythm.
- C. sinus bradycardia.
- D. atrial fibrillation.
Answer:
D
Explanation:
Mitral stenosis leads to increased pressure in the left atrium, which can cause atrial enlargement and
predispose patients to atrial fibrillation. Atrial fibrillation is the most common arrhythmia associated
with mitral stenosis due to the structural changes in the atrium. Reference: = CCRN Exam Handbook
and AACN's Certification Review Course materials.
Question 8
For a patient who sustained blunt renal trauma and a crush injury to the leg, monitoring should
include observing for
- A. a shortened PR interval.
- B. tall peaked T waves.
- C. ST segment depression.
- D. a prolonged PR interval.
Answer:
B
Explanation:
Crush injuries can lead to significant muscle damage and rhabdomyolysis, resulting in the release of
intracellular potassium into the bloodstream, causing hyperkalemia. Tall peaked T waves are a classic
sign of hyperkalemia, which needs to be closely monitored in these patients. Reference: = CCRN
Exam Handbook and AACN's Certification Review Course materials.
Question 9
An unconscious patient presents with the following laboratory values: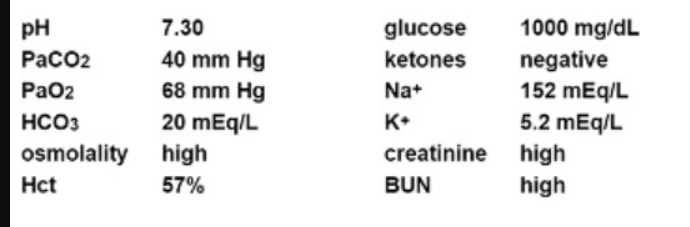
Appropriate management of this patient should include
- A. IV hydration.
- B. hemodialysis.
- C. intubation.
- D. osmotic diuresis.
Answer:
A
Explanation:
The laboratory values indicate hyperosmolar hyperglycemic state (HHS), characterized by high
glucose levels, high osmolality, and dehydration. The primary management includes aggressive IV
hydration to correct dehydration and improve circulation. Hemodialysis and intubation are not
immediate priorities unless there are other indications, and osmotic diuresis is not appropriate in
this context. Reference: = CCRN Exam Handbook and AACN's Certification Review Course materials.
Question 10
In a patient with status asthmaticus, which of the following indicate a deteriorating condition?
- A. increased compliance and respiratory acidosis
- B. increased PaCO2 and decreased expiratory flow
- C. respiratory alkalosis and increased expiratory flow
- D. decreased PaCO2 and increased minute ventilation
Answer:
B
Explanation:
In status asthmaticus, a worsening condition is indicated by increased PaCO2 and decreased
expiratory flow. This reflects severe airway obstruction and ventilatory failure, leading to hypercapnia
(elevated PaCO2) and a decrease in the ability to exhale effectively. Reference: = CCRN Exam
Handbook and AACN's Certification Review Course materials.
Question 11
The rationale for initiating early enteral feeding in a patient with sepsis is to
- A. minimize translocation of GI bacteria.
- B. minimize electrolyte imbalances and fluid shifts.
- C. prevent pulmonary aspiration.
- D. increase GI motility.
Answer:
A
Explanation:
Early enteral feeding in patients with sepsis is crucial as it helps maintain gut integrity, thereby
minimizing the translocation of gastrointestinal (GI) bacteria. The presence of nutrients in the gut
lumen supports the mucosal barrier function and reduces bacterial translocation, which can lead to
secondary infections and further complications in septic patients. Reference: = CCRN Exam
Handbook and AACN's Certification Review Course materials.
Question 12
A patient underwent bariatric surgery for weight loss 3 days ago. The patient appears anxious,
restless, and reports increased abdominal pain over the last 24 hours. The nurse palpates mild
subcutaneous crepitus over the neck. Vital signs are:
BP 106/64
HR 128
RR 27
T 100.4° F (38°C)
Which action should the nurse anticipate?
- A. Obtain labs.
- B. Administer a 1000 mL bolus of normal saline.
- C. Provide broad spectrum antibiotics.
- D. Prepare the patient for surgery.
Answer:
D
Explanation:
The signs and symptoms described in the patient post-bariatric surgery, including anxiety,
restlessness, increased abdominal pain, and subcutaneous crepitus over the neck, suggest a potential
anastomotic leak, which is a surgical emergency. Given the vital signs indicating possible sepsis or
shock (elevated heart rate, increased respiratory rate, and fever), immediate surgical intervention is
likely required to repair the leak and prevent further complications. Reference: CCRN Exam
Handbook, AACN, page 30, section on GI surgical emergencies.
Question 13
The primary pathophysiology underlying acute respiratory failure in a patient with head trauma
involves
- A. hypercapnia related to decreased minute ventilation.
- B. shifting of oxyhemoglobin dissociation curve to the left.
- C. increased arterial oxygenation related to increased intrapulmonary shunt.
- D. dehydration related to diabetes insipidus.
Answer:
A
Explanation:
In a patient with head trauma, the primary pathophysiology underlying acute respiratory failure
often involves hypercapnia due to decreased minute ventilation. Head trauma can impair the central
nervous system's ability to regulate breathing, leading to inadequate ventilation and a build-up of
carbon dioxide (CO2) in the blood. Other factors like shifting of the oxyhemoglobin dissociation
curve, increased intrapulmonary shunt, and dehydration due to diabetes insipidus may be present
but are not the primary causes. Reference: CCRN Exam Handbook, AACN, page 25, section on
Respiratory.
Question 14
Which of the following is the most common prerenal cause of acute tubular necrosis?
- A. shock
- B. blood transfusion reaction
- C. crush injury
- D. beta-hemolytic streptococcal infection
Answer:
A
Explanation:
Shock is the most common prerenal cause of acute tubular necrosis (ATN). In the context of prerenal
conditions, shock leads to decreased renal perfusion and subsequent ischemia, which can cause
damage to the renal tubules. Other options such as blood transfusion reaction, crush injury, and
beta-hemolytic streptococcal infection can lead to renal damage but are not the most common
prerenal causes of ATN. Reference: CCRN Exam Handbook, AACN, page 28, section on Renal/GU.
Question 15
Family members have been complaining about limited visiting hours. To facilitate a potential change
in practice, a nurse should first
- A. schedule an interdisciplinary team meeting to discuss visiting hours.
- B. begin a literature search on family visitation practices.
- C. consult with medical staff to change visiting hours.
- D. draft a new policy regarding visitation practices for the unit.
Answer:
B
Explanation:
The initial step in facilitating a change in practice regarding visiting hours should involve a literature
search on family visitation practices. This allows the nurse to gather evidence-based information that
can support any proposed changes. After gathering sufficient evidence, the nurse can then schedule
an interdisciplinary team meeting to discuss the findings, consult with medical staff, and draft a new
policy if necessary. Reference: CCRN Exam Handbook, AACN, page 35, section on Professional Caring
and Ethical Practice.